Autonomic dysfunction represents a complex group of conditions that affect the autonomic nervous system, which regulates essential functions such as heart rate, blood pressure, digestion, and temperature control.
For patients experiencing persistent and unexplained symptoms, finding a clear diagnostic path can be challenging, and many are referred to a dysautonomia treatment specialist early in their care journey, even when traditional tests appear normal.
Recent advances in neurological imaging are changing this landscape by offering deeper insights into the structure and function of the autonomic nervous system in health and disease.
Understanding the Role of Imaging in Autonomic Disorders
Neurological imaging plays a critical role in ruling out structural causes of autonomic symptoms and identifying subtle abnormalities that may not be visible through routine testing.
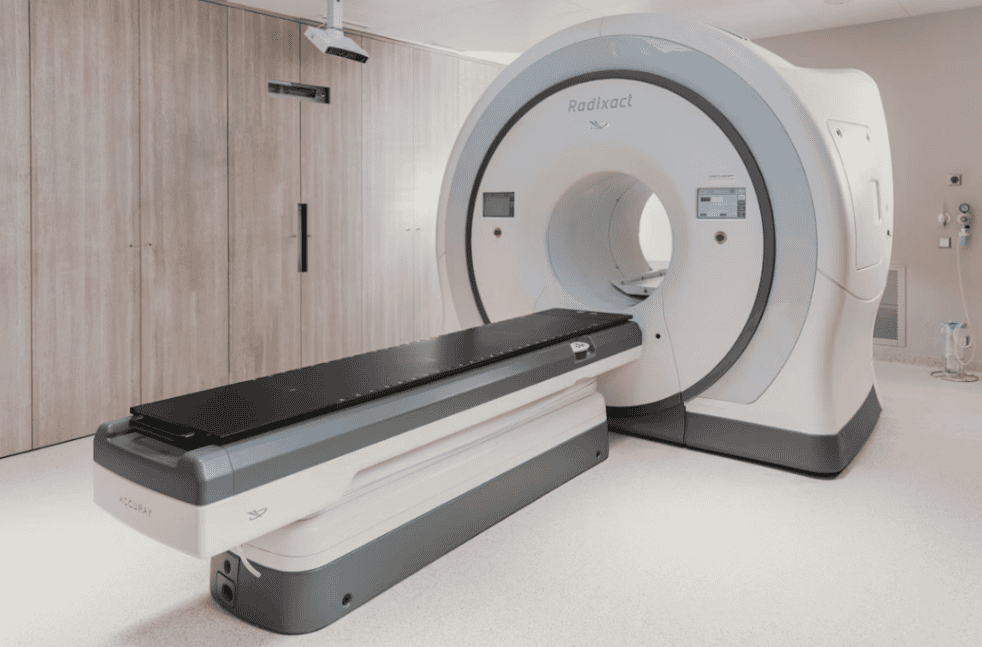
Traditional imaging techniques, such as standard magnetic resonance imaging, have long been used to assess the brain and spinal cord for lesions, tumors, or degenerative changes that could disrupt autonomic pathways. While these scans often appear normal in autonomic dysfunction, they provide an essential baseline for further investigation.
Advances in imaging technology now allow clinicians to go beyond gross anatomy and explore functional and microstructural changes. High-resolution MRI techniques can detect small alterations in brainstem regions and autonomic control centers that were previously difficult to visualize.
These developments help clinicians better understand why patients experience symptoms such as dizziness, fainting, or abnormal heart rate regulation despite unremarkable conventional scans.
Functional Imaging and Autonomic Regulation
Functional neurological imaging has opened new possibilities for studying how the autonomic nervous system responds to stress, posture, and physiological challenges.
Functional MRI enables researchers to observe changes in blood flow associated with neural activity in regions responsible for autonomic control. This approach provides insight into how communication between the brain and peripheral autonomic nerves may be altered in dysfunction.
By examining these functional patterns, clinicians can begin to correlate specific symptoms with disrupted neural networks. For example, altered activation in areas involved in cardiovascular regulation may help explain orthostatic intolerance or abnormal blood pressure responses.
Although functional imaging is still primarily used in research settings, it is steadily contributing to a more nuanced understanding of autonomic disorders.
Advanced Imaging Techniques and Emerging Research
Diffusion-based imaging techniques are also contributing valuable information about autonomic dysfunction. These methods assess the integrity of white matter pathways that carry signals between the brain, spinal cord, and autonomic ganglia. Subtle disruptions in these pathways may help explain the widespread and multisystem nature of autonomic symptoms.
In addition, research into molecular and metabolic imaging is shedding light on neurochemical changes associated with autonomic disorders. While still evolving, these approaches may eventually enable clinicians to identify patterns associated with inflammation, altered neurotransmitter activity, or impaired cellular metabolism.
As this research progresses, imaging could play a greater role in guiding personalized management strategies rather than serving solely as a diagnostic exclusion tool.
Clinical Impact and Future Directions
The integration of advanced neurological imaging into clinical practice has the potential to improve diagnostic confidence for both clinicians and patients. When imaging findings align with clinical symptoms and physiological testing, patients may feel more validated and better informed about their condition. This alignment can also support earlier intervention and more targeted care planning.
Looking ahead, continued collaboration between neurologists, imaging specialists, and researchers will be essential. As imaging techniques become more refined and accessible, they may help bridge the gap between symptom-based diagnosis and objective evidence in the assessment of autonomic dysfunction. These advances point toward a future where imaging not only enhances understanding but also directly informs treatment decisions.
Conclusion
Neurological imaging has evolved from a tool used primarily to exclude major pathology into a powerful means of exploring the complex mechanisms underlying autonomic dysfunction.
Advances in structural, functional, and diffusion imaging are gradually revealing how subtle neural changes can lead to significant clinical symptoms.
As research continues and technology advances, imaging is likely to play an increasingly important role in improving diagnosis, understanding disease mechanisms, and supporting more effective care for individuals living with autonomic disorders.