Medical malpractice cases are labyrinthine journeys through the interplay of healthcare systems, professional standards, and patient outcomes. At the core of many such claims lies the question of negligence. What constitutes medical negligence, and how does it affect patient care?
This post dives into the complexities of negligence in the context of medical malpractice, shedding light on the nuances that impact the healthcare narrative.
Understanding Medical Negligence
At its essence, medical negligence refers to the omission or commission of an act by a healthcare provider that deviates from the accepted standard of care, leading to injury or death to the patient.
Key to this definition is the concept of ‘standard of care’, a benchmark against which the provider’s actions are measured. This is not a static yardstick but a constantly evolving set of practices informed by medical advancements and professional consensus.
The crux of any medical negligence claim is establishing that a healthcare provider breached the standard of care. As the experts from Hoover medical malpractice law explain, this involves demonstrating that the provider failed to act as a reasonably prudent healthcare professional would under similar circumstances. Proving this breach often requires expert testimony to dissect the specifics of the medical situation and the actions of the provider.
The Puzzle of Proving Negligence
For a patient or their legal representative, the path to proving medical negligence can resemble a complex puzzle. It involves gathering evidence, analyzing medical records, and consulting with experts who can provide a professional opinion on the standard of care and its breach. Each piece of the puzzle is critical, and the process can often be time-consuming and emotionally taxing for all parties involved. By understanding POA in Washington State, individuals can ensure that the right person is legally empowered to make medical decisions or pursue legal action on behalf of a patient when necessary. Establishing a clear power of attorney early on can prevent confusion and protect the patient’s rights throughout the legal process.
Factors Influencing Negligence Claims
Negligence in medical malpractice cases can be influenced by a myriad of factors, many of which are industry-specific and highly technical.
1. Informed Consent and Communication
One crucial aspect is the presence or absence of informed consent. Healthcare providers have a duty to communicate information to patients in a way that allows them to make educated decisions about their care. A failure to adequately inform patients about risks and alternatives can factor into a negligence claim.
Effective communication in healthcare is multifaceted. It encompasses not only the exchange of information but also the ability to comprehend and respond to patient concerns and questions. When miscommunication or a lack of it leads to poor outcomes, negligence claims often follow.
2. Documentation and Record Keeping
Accurate and timely documentation is the backbone of healthcare, and it’s no less critical in the context of medical malpractice defense. Not only can detailed records demonstrate that the standard of care was met, but the absence of such documentation can also raise red flags and support the patient’s claim of negligence.
Proper record-keeping practices involve more than just noting down what occurred. They should paint a clear picture of the patient’s history, diagnosis, treatment plan, and the reasoning behind decisions made. In the absence of this clarity, a negligence claim can gain significant traction.
3. Organizational Policies and Practices
Negligence can extend beyond the actions of an individual provider to the policies and practices of the organization. For instance, if a hospital fails to ensure that its staff is adequately trained or does not have appropriate systems in place to prevent errors, it can be found liable for negligence.
Organizational liability is particularly relevant in cases involving systemic failures such as medication errors due to faulty systems, lack of follow-up care, or issues related to health record management. Identifying and holding organizations accountable for their role in medical malpractice is a growing aspect of negligence claims.
The Human Dimension of Negligence
Medical negligence is not just a legal concept; it’s deeply human. It involves the suffering of patients who sought care and ended up worse off.
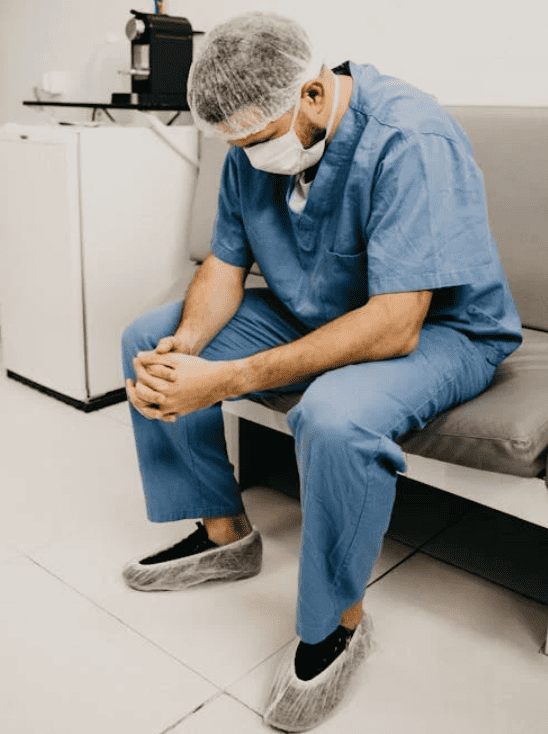
Emotional and Psychological Impact
The emotional and psychological impacts of perceived negligence can be profound. Patients may experience a loss of trust in the medical profession as a whole or the specific providers involved. These feelings of betrayal or abandonment can complicate the patient’s recovery and well-being, underscoring the significance of negligence claims beyond the financial compensation they may bring.
Impact on the Healthcare System
Negligence claims also have a broader impact on the healthcare system. Rising malpractice premiums can lead to increased healthcare costs and the defensive practice of over-prescription and over-diagnosis to protect against potential claims. It’s an intricate feedback loop where the threat of negligence claims can actually influence the standard of care itself.
Professional and Ethical Considerations
For healthcare providers, being accused of negligence can be a harrowing experience. It not only affects their professional reputation but also raises profound ethical questions about their role in the patient’s outcome.
The implications of a negligence claim go beyond individual providers to the professional community at large. They can lead to a reevaluation of protocols and practices and potentially set new precedents for what constitutes the standard of care in specific circumstances.
Beyond Negligence: Reshaping the Narrative
The discourse around medical malpractice is often focused on the legal aspects, but the story is much broader. It’s about the intersection of technology and humanity, of professionalism and compassion. It’s about reshaping the narrative to ensure that negligence is not just a term of the courtroom but a concept that continues to refine and improve the delivery of healthcare.
In this narrative, patients are not just litigants but stakeholders in their care. Providers are not just practitioners but part of a larger system that must balance the complexities of delivering care with the imperative of doing no harm.
The role of negligence in medical malpractice is multifaceted, mirroring the complexities of the healthcare system itself. It stands at the crossroads of law, ethics, and patient care, highlighting the profound impact that a breach in the standard of care can have.
By understanding the intricacies of medical negligence, stakeholders in the healthcare community can work towards a system that not only addresses claims but, more importantly, improves patient outcomes and upholds the sanctity of care.