Understanding the Types of Solid Tumors in Oncology Practice
Solid tumors represent a significant portion of cancer diagnoses globally and pose complex challenges to oncology professionals. Unlike hematologic malignancies, solid tumors originate in tissues or organs and form a mass, often requiring a multifaceted treatment approach.
For healthcare professionals (HCPs), a deep understanding of types of solid tumors is essential for accurate diagnosis, treatment planning, and care coordination. Furthermore, leveraging comprehensive Oncology Resources can optimize outcomes and align clinical decisions with the latest evidence-based practices.
What Are Solid Tumors?
Solid tumors are abnormal masses of tissue that typically do not include cysts or liquid areas. They differ fundamentally from hematologic cancers (e.g., leukemia, lymphoma), which affect the blood, bone marrow, or lymphatic system. Solid tumors can be benign (non-cancerous) or malignant (cancerous), with malignancies requiring prompt and often aggressive intervention.
Common Types of Solid Tumors
Solid tumors are generally categorized based on the tissue of origin. This classification helps guide diagnostics, prognostic evaluation, and therapy selection.
Carcinomas
Carcinomas are the most prevalent type, originating from epithelial cells lining organs and body surfaces. Common examples include:
- Breast carcinoma
- Colorectal carcinoma
- Lung carcinoma
- Prostate carcinoma
According to the American Cancer Society (ACS), carcinomas account for over 80% of all cancer diagnoses in the U.S.
Sarcomas
Sarcomas arise from connective tissues such as bone, muscle, fat, or cartilage. Though rare, they are aggressive and include:
- Osteosarcoma (bone)
- Liposarcoma (fat)
- Leiomyosarcoma (smooth muscle)
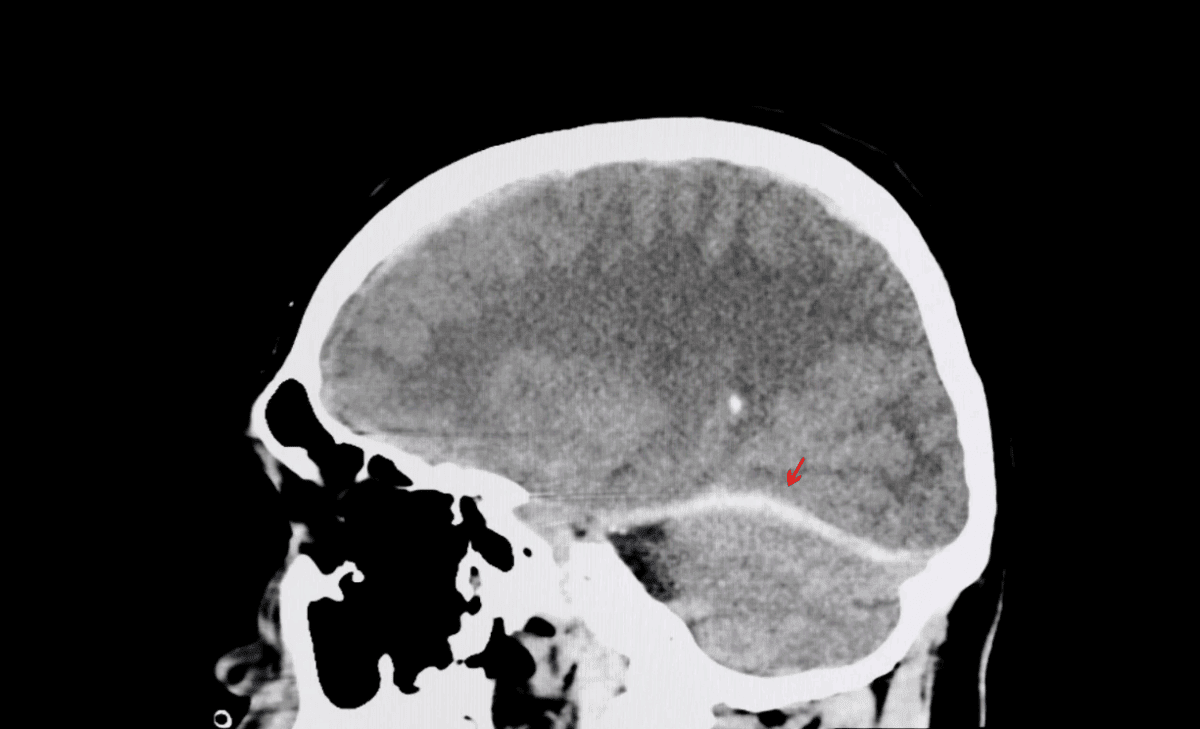
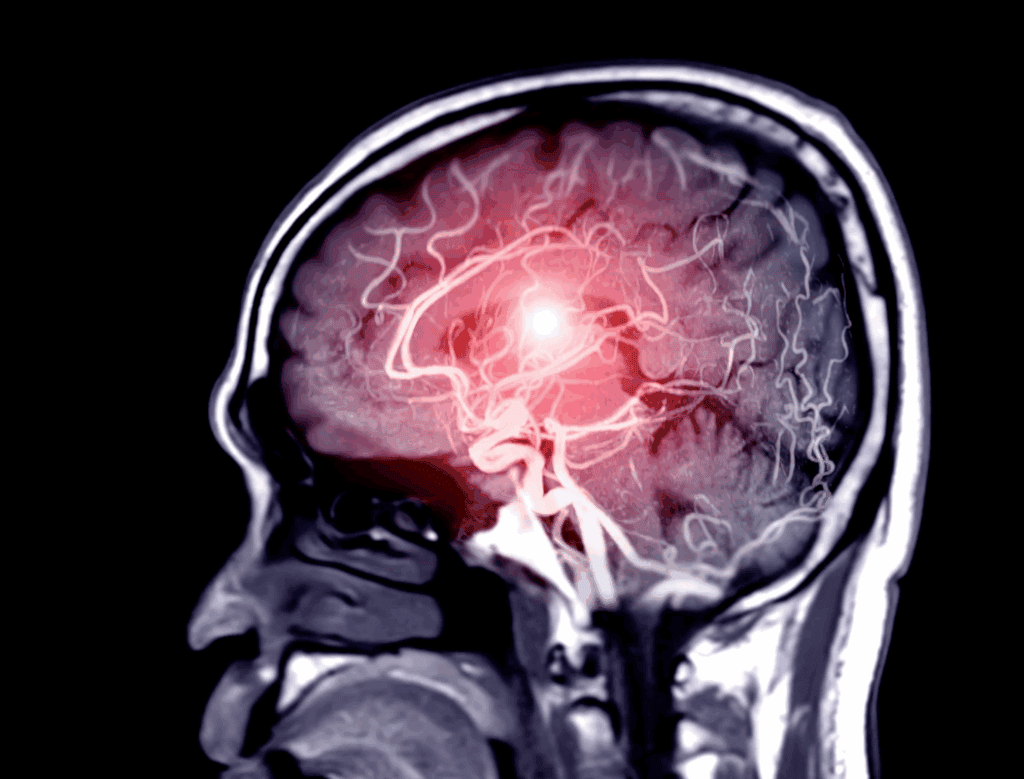
Central Nervous System Tumors
These tumors affect the brain and spinal cord. Glioblastoma multiforme, one of the most aggressive forms, has a median survival of just over 15 months despite aggressive treatment.
Germ Cell Tumors
Typically affecting the testes or ovaries, these tumors are most common in adolescents and young adults. Many are curable with cisplatin-based chemotherapy.
Epidemiology and Burden
Cancer remains the second leading cause of death in the U.S. According to the Centers for Disease Control and Prevention (CDC), nearly 1.9 million new cancer cases were diagnosed in 2023, with solid tumors making up the vast majority. Lung and bronchus cancers account for 12% of all new cases, followed closely by breast (female) and prostate cancers.
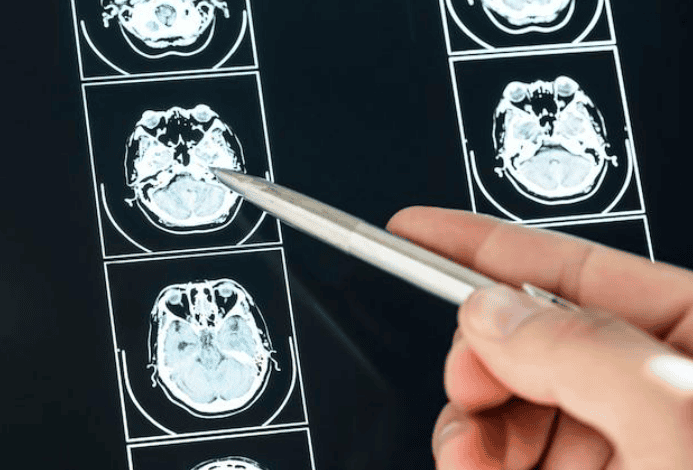
Diagnostic Pathways and Staging
Diagnosis of solid tumors typically involves a combination of imaging (MRI, CT, PET), histopathologic examination via biopsy, and molecular profiling. Tumor staging—using systems like TNM—assesses the size, lymph node involvement, and metastasis, which are critical for prognosis and treatment strategy.
Treatment Modalities for Solid Tumors
Treatment plans are often multimodal and tailored to tumor type, stage, patient performance status, and biomarker profile.
Chemotherapy
Cytotoxic chemotherapy remains a mainstay for many solid tumors, especially in adjuvant or metastatic settings. Despite side effects, it plays a crucial role in reducing tumor burden and improving survival.
Immunotherapy and Targeted Agents
The past decade has seen remarkable advances in immunotherapy (e.g., checkpoint inhibitors like pembrolizumab) and targeted therapies that disrupt cancer-specific pathways. For example, HER2-positive breast cancer responds well to trastuzumab and other HER2-targeting agents, improving progression-free survival substantially.
The Role of Biomarkers in Solid Tumor Management
Biomarkers such as PD-L1 expression, EGFR mutations, and BRCA1/2 status enable tailored treatment. They are increasingly critical for selecting patients likely to benefit from immunotherapies or targeted agents. Biomarker testing is now standard of care in many solid tumors, including non-small cell lung cancer and metastatic colorectal cancer.
Challenges in Treating Advanced Solid Tumors
Despite therapeutic advances, significant challenges remain. Tumor heterogeneity and acquired resistance often limit the efficacy of systemic therapies. The tumor microenvironment, immune evasion, and drug delivery barriers contribute to poor outcomes in certain advanced cancers.

Integrating Oncology Resources into Clinical Practice
Access to trusted Oncology Resources is vital for staying current with evolving guidelines, drug approvals, and trial opportunities. These resources include:
- National Comprehensive Cancer Network (NCCN) Guidelines
- American Society of Clinical Oncology (ASCO) Recommendations
- ClinicalTrials.gov for enrolling patients in ongoing studies
- SEER Program Data from the National Cancer Institute (NCI)
Healthcare professionals who actively consult these resources can make more informed, evidence-aligned decisions, ultimately improving patient outcomes.
Multidisciplinary Care and Support Services
A team-based approach is essential in oncology. Tumor boards, involving oncologists, radiologists, pathologists, and palliative care specialists, ensure comprehensive management. Support services such as nutrition, social work, and mental health counseling address the broader needs of patients and families.
Emerging Trends and Future Outlook
Precision oncology, artificial intelligence (AI)-driven diagnostics, and real-world evidence are reshaping the future of solid tumor care. Liquid biopsies offer non-invasive options for monitoring tumor progression and treatment response, while AI tools are enhancing radiologic and pathologic assessments.
Clinical trial designs are also evolving to include adaptive and basket trials, expanding access for patients with rare mutations across different tumor types.
Conclusion
Understanding the full spectrum of types of solid tumors is foundational for delivering personalized and effective oncology care. With the growing complexity of treatment modalities and the emergence of precision medicine, it is imperative that HCPs harness credible Oncology Resources to inform clinical decisions.
By integrating diagnostics, therapeutic advances, and supportive care into a patient-centered framework, clinicians can elevate both survival and quality of life for individuals facing solid tumor diagnoses.