Discovering you are pregnant brings a mix of emotions, from excitement to trepidation. One aspect of early pregnancy that can cause a fair bit of discomfort is morning sickness, a common condition characterized by nausea and vomiting.
Understanding when this condition typically begins and how to manage it can greatly improve a pregnant individual’s quality of life. Below, we delve into the intricacies of the onset of morning sickness, providing insights and advice to help navigate this challenging phase.
Understanding the Onset of Morning Sickness: An Overview
Morning sickness is a misnomer, as the associated nausea and vomiting can occur at any time of the day or night. It usually starts around the sixth week of pregnancy, but for some, it can begin as early as four weeks. From mild discomfort to severe episodes that interfere with daily life, the intensity of symptoms varies greatly from person to person.
Many expectant mothers find themselves eager for information regarding morning sickness. Questions like, “When does morning sickness start?” often dominate early pregnancy discussions. Typically, this condition lasts until the end of the first trimester, but for some, it might persist longer.
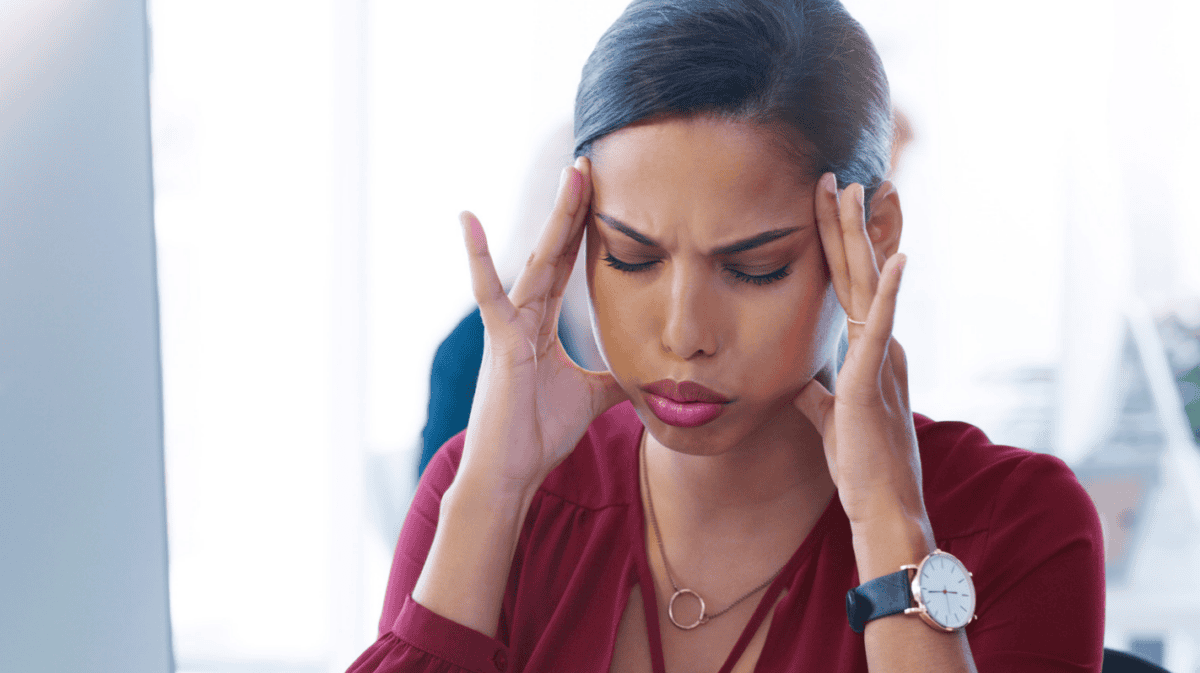
The emotional impact of morning sickness should not be underestimated. Coping with constant nausea can be mentally exhausting and can affect one’s mood and outlook. The anticipation of relief as the pregnancy progresses does provide a psychological boost for many.

The Biological Mechanisms Behind Morning Sickness
At the core of morning sickness is the body’s adaptive response to pregnancy. The surge of hCG and other hormones is considered to protect the fetus during a critical period of development. It is hypothesized that nausea is a way of ensuring pregnant individuals avoid foods that could harbor toxins or pathogens that might harm the embryo.
Digestive alterations are another facet of the body’s protective measures as it adapts to nurturing the growing fetus. Slower digestion ensures better absorption of nutrients, but this can also lead to the discomfort associated with morning sickness. The heightened sense of smell experienced during pregnancy can also trigger waves of nausea.
Research has pointed to additional physiological factors that may influence morning sickness. The placenta, as it develops, produces a variety of substances that affect the mother’s metabolism and possibly her gastrointestinal system. However, these mechanisms are complex and continue to be the subject of study.
Managing Morning Sickness: Strategies for Relief and Comfort
Managing morning sickness involves a combination of dietary changes, lifestyle adjustments, and sometimes medication. Eating small, frequent meals throughout the day instead of large portions can help. Opting for bland foods that are easy on the stomach is also generally recommended.
Keeping hydrated is essential, but it can be challenging when feeling nauseous. Sipping on water or sucking on ice chips throughout the day can help maintain fluid levels. Some find relief in ginger in various forms, such as tea or candy, which has natural anti-nausea properties.
Lifestyle modifications, such as ensuring adequate rest, can be beneficial. Avoiding strong odors and ensuring good ventilation often helps reduce nausea triggers. For some, acupressure or acupuncture provides symptom relief as well.

When to Seek Medical Advice for Morning Sickness Concerns
While morning sickness is typically not dangerous, it’s important to monitor the severity of symptoms. If nausea and vomiting prevent adequate intake of food and fluids, it could lead to dehydration and weight loss, both of which can be harmful to both the mother and the developing baby.
In severe cases, a condition known as hyperemesis gravidarum can occur, where the vomiting is excessive and may require hospitalization. Symptoms of this condition include constant nausea that doesn’t subside, severe vomiting, dehydration, and an inability to keep down any food or drink. Prompt medical attention is necessary in these cases.
Lastly, mental and emotional support is key. If morning sickness is affecting mental health, talking to a counselor or joining a support group can provide coping strategies and an additional layer of support.
Altogether, morning sickness is a common pregnancy ailment with various contributing factors and potential management strategies. Understanding its biological mechanisms, reflective triggers, and relief methods can empower pregnant individuals to navigate this challenging time. Overall, it’s important to maintain open communication with healthcare providers to manage symptoms effectively and secure the best possible outcome for both the mother and the growing baby.