Over one-third of medical claims in the U.S. are initially denied, and urgent care centers are among the hardest hit because of speed-driven mistakes. Every missed modifier, every incomplete chart, and every coding shortcut quietly drains revenue from clinics that are already stretched thin.
Urgent care was built for momentum. Patients walk in without warning. Providers move quickly. Front desks stay packed. In that constant motion, billing often becomes an afterthought, and that’s where profits start slipping away.
Outsourcing urgent care billing services is no longer a back-office convenience. For many high-volume clinics, it has become a financial survival strategy.
The Revenue Strain Unique to Urgent Care Clinics
Urgent care is unlike any other outpatient model. There are no long appointment blocks, no predictable treatment paths, and no consistent payer mix. One shift may include workers’ compensation visits, pediatric fevers, lacerations, imaging, injections, and chronic flare-ups, each with its own billing structure.
This variety creates complexity. Coders must apply the right CPT and ICD-10 codes under time pressure. Front-office teams must verify insurance in minutes, not hours. Providers must document thoroughly when moving patients to other patients.
When even one step breaks down, claims stall, denials rise, and revenue leaks quietly month after month.
Why In-House Billing Often Falls Short?
Most urgent care centers didn’t open with the goal of becoming billing operations. Yet many still rely on a small internal team to manage coding, claim submission, follow-ups, appeals, compliance, reporting, and patient billing.
That’s an enormous workload.
Turnover is common. Training takes time. Regulations change yearly. Payers revise reimbursement rules constantly. A single understaffed billing department can’t always keep pace, and urgent care clinics feel the effects quickly through delayed cash flow and rising accounts receivable.
Outsourcing doesn’t replace internal control. It reinforces it with depth, scale, and specialization.
How Outsourcing Directly Increases Collected Revenue
1. Specialized Coders Capture What Busy Clinics Miss
Urgent care encounters are detail-heavy. Time-based codes, bundled services, injections, imaging, supplies, and evaluation levels all affect reimbursement.
Outsourced teams employ coders who work only within healthcare revenue systems. They monitor annual CPT updates, payer policy changes, and modifier requirements. Their job is not multitasking; it is precision.
That precision reduces under-coding, prevents over-coding risks, and increases first-pass acceptance. More clean claims mean faster payments and fewer write-offs.
2. Denials Become Recovery Opportunities Instead of Dead Ends
Denied claims don’t have to mean lost income, but only if someone has the time and expertise to pursue them.
External billing teams track denial trends, identify payer behavior patterns, correct documentation gaps, and aggressively appeal where appropriate. They don’t simply resubmit. They analyze.
This turns billing from a passive task into an active revenue recovery process. Many urgent care clinics see measurable gains simply from professional denial management alone.
3. Overhead Shrinks While Financial Output Grows
Maintaining an in-house billing department means salaries, benefits, turnover risk, training, compliance education, and software subscriptions. When volume spikes or staff leave, performance drops.
Outsourced billing converts those unpredictable internal costs into a stable operational expense. Clinics pay for performance, not payroll fluctuation.
That financial consistency allows leadership to plan growth, invest in equipment, extend hours, or open new locations without worrying about whether the billing department can keep up.
4. Better Technology Without Heavy Investment
Modern billing partners operate on advanced revenue cycle platforms that many small or mid-sized clinics can’t justify purchasing alone.
These systems scrub claims before submission, flag coding inconsistencies, track aging accounts, and produce detailed financial reports. Administrators can see payer turnaround times, denial reasons, reimbursement gaps, and month-to-month performance trends.
Instead of guessing where revenue is going, urgent care owners finally gain visibility and visibility drives control.
5. Compliance Stops Being a Constant Fear
Urgent care billing services operates under serious legal oversight. HIPAA governs data handling. CMS sets reimbursement policies. State regulations affect workers’ compensation, urgent care licensing, and payer contracting.
Outsourced billing firms are built around compliance. Their workflows are designed to protect patient data, document services accurately, and meet audit standards. Many employ certified billing and coding professionals who track regulatory changes as part of their daily role.
That protection reduces the risk of audits, penalties, and reputation damage risks that no clinic can afford.
What Real Clinics Experience After Outsourcing
Urgent care operators who shift billing externally often report the same changes:
• Fewer denied claims
• Shorter payment cycles
• Lower accounts receivable days
• Clearer financial reporting
• Less staff burnout
• Improved front-desk efficiency
One regional clinic group struggling with rising denials and delayed reimbursements reported a dramatic improvement within the first two quarters after outsourcing. Claims stopped aging. Revenue stabilized. Administrative teams returned their focus to patients rather than payer portals.
The financial relief extended beyond money. It restored operational breathing room.
How to Choose the Right Outsourcing Partner
Not all billing services understand urgent care. Clinics should look beyond price and evaluate:
• Experience specifically within urgent care environments
• Transparent performance reporting
• Proven denial management processes
• HIPAA-aligned data security systems
• Scalable support for multi-location growth
• Responsive communication channels
A strong partner does not function as a vendor. They operate as a financial extension of the clinic.
Common Fears That Hold Clinics Back
Some owners worry that outsourcing means losing control. In practice, it often creates more oversight through structured reporting and accountability.
Others fear a higher cost. Yet many clinics recover more in underpaid or denied claims than the service fee itself.
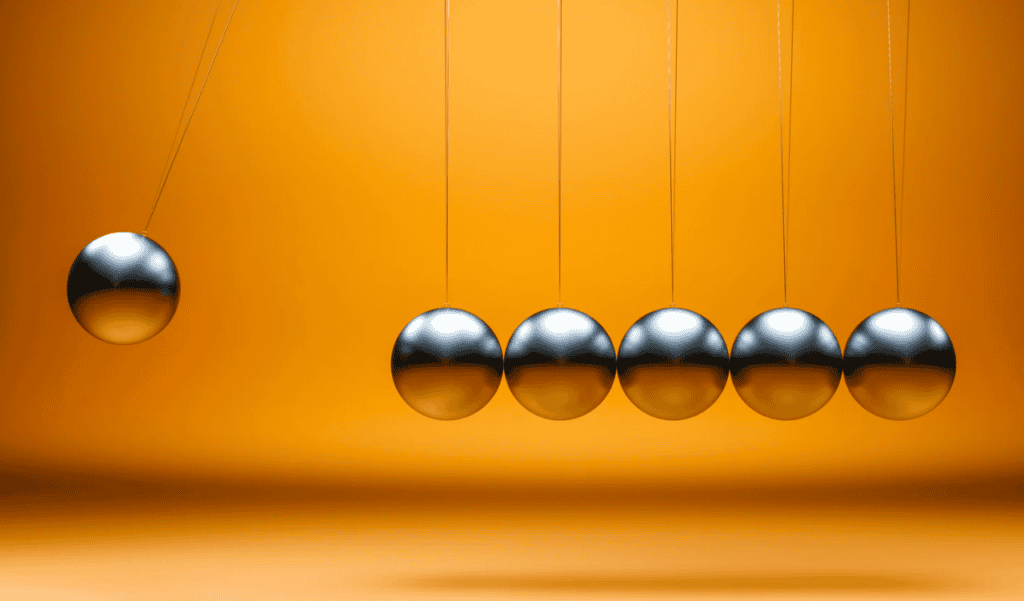
The real risk isn’t outsourcing. It’s continuing to operate a revenue engine that quietly loses money every day.
The Direction of Urgent Care Billing Is Moving
Healthcare reimbursement is becoming more performance-driven, more data-dependent, and more compliance-sensitive. As telehealth, occupational medicine, and value-based reimbursement expand, billing accuracy becomes even more critical.
Clinics that align with specialized billing operations today are better positioned to adapt tomorrow without overloading internal teams.
Final Word
Urgent care clinics are built for speed, accessibility, and patient flow. Their billing systems should match that same level of efficiency.
Outsourcing allows clinics to protect revenue, stabilize cash flow, reduce internal strain, and operate with financial clarity. When done correctly, it doesn’t change how urgent care functions; it strengthens it.
For clinics seeking to reclaim lost income, reduce denials, and build long-term financial consistency, partnering with experienced urgent care billing services may be the smartest operational decision they make.