Emergencies can happen at any time. Whether it’s a fall, a medical crisis, or a security threat, having a way to call for help quickly can make all the difference. Emergency call buttons provide an instant connection to assistance, ensuring that people receive the help they need when they need it most. These devices have become a crucial part of personal safety, particularly for seniors, individuals with medical conditions, and workers in high-risk environments.
Despite their small size, emergency call buttons play a massive role in saving lives. They are easy to use and can be activated with a simple press. But how exactly do they work? What types are available, and who benefits the most from them?
This article explores these questions about the role of emergency call buttons, shedding light on the importance of these life-saving devices.
Why Emergency Call Buttons Matter
The need for emergency response systems has never been greater. As populations age and more people live independently, the risk of being alone during an emergency increases. This is especially true for seniors who may experience falls or sudden health issues. Immediate access to help can prevent a minor incident from becoming a life-threatening situation.
For those in Canada, life alert Canada offers a reliable way to summon assistance at the press of a button. Whether it’s a senior living alone or a worker in a hazardous job, these systems ensure help is always within reach. They provide peace of mind to users and their loved ones, knowing that emergencies won’t go unnoticed.

How Emergency Call Buttons Work
Emergency call buttons operate on a simple principle—pressing a button sends an alert to a designated responder. This could be a family member, a 24/7 monitoring center, or emergency services, depending on the system in place.
Key Features of Emergency Call Systems
- Instant Alerts: The button sends a signal immediately after being pressed, ensuring there’s no delay in getting help.
- Wireless Connectivity: Many modern systems use wireless technology, allowing users to move freely without losing connection.
- Two-Way Communication: Some models come with built-in speakers and microphones, enabling direct communication with responders.
- Automatic Fall Detection: Advanced models can detect falls automatically, triggering an alert even if the user is unable to press the button.
- GPS Tracking: Mobile units with GPS help locate users in real-time, which is especially useful for active seniors and outdoor workers.
Different Types of Emergency Call Buttons
Not all emergency call buttons are the same. They come in various forms to suit different needs and environments.
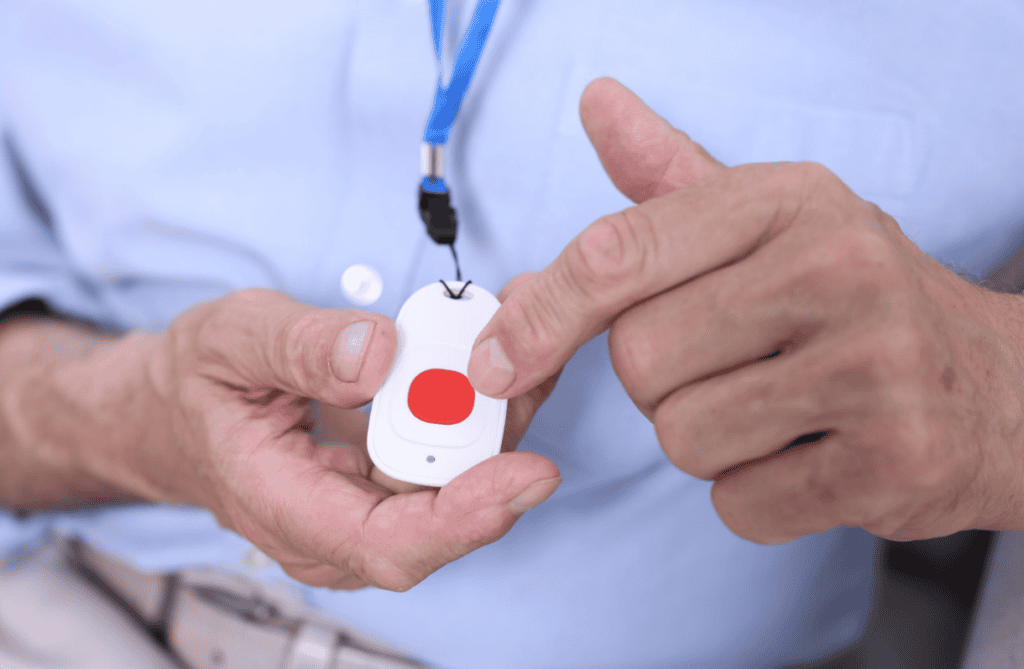
1. Wearable Emergency Buttons
Wearable emergency buttons are the most common type. They are often worn as pendants or wristbands, ensuring they are always within reach. These devices are lightweight, waterproof, and designed for everyday use.
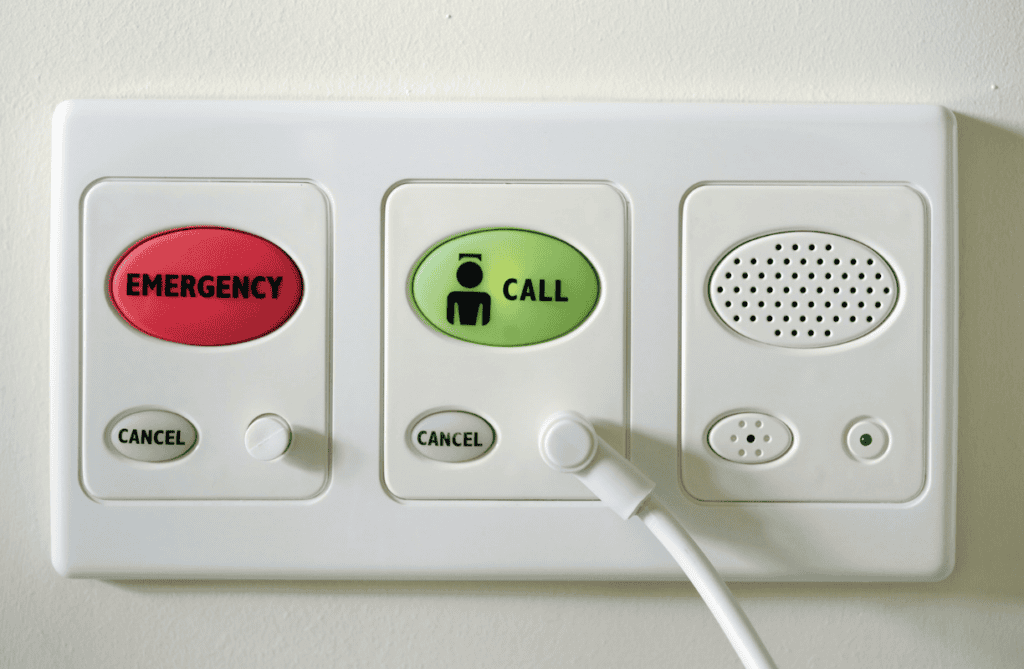
2. Wall-Mounted Emergency Buttons
Wall-mounted buttons are ideal for locations where falls or emergencies are more likely to occur, such as bathrooms, staircases, and kitchens. These fixed buttons ensure that assistance can be requested even if a wearable device is out of reach.
3. Mobile Emergency Call Devices
Unlike home-based systems, mobile emergency buttons work anywhere there is cellular coverage. These are great for people who travel frequently or spend time outdoors. GPS tracking ensures responders can locate the user even if they cannot communicate their location.
4. Workplace Emergency Call Systems
Certain industries require emergency call buttons to protect employees working in high-risk conditions. These include lone worker devices, which allow employees in remote or hazardous locations to summon help quickly.
Who Benefits the Most from Emergency Call Buttons?
Emergency call buttons are valuable for various groups of people. While they are most commonly associated with seniors, they serve a much broader audience.
1. Seniors Living Alone
Older adults who live independently are at higher risk of medical emergencies and falls. An emergency button allows them to maintain independence while ensuring they can get help if needed.
2. Individuals with Medical Conditions
People with chronic illnesses, mobility challenges, or conditions like epilepsy or heart disease benefit from having a quick way to call for assistance. These buttons reduce response time in case of a medical emergency.
3. Caregivers and Family Members
Emergency call systems provide peace of mind to caregivers and families, knowing their loved ones can get help even when they are not physically present.
4. Workers in High-Risk Jobs
Lone workers, construction workers, and people in hazardous industries need a way to call for help in case of an accident. Some emergency buttons are specifically designed for workplace safety.
Choosing the Right Emergency Call Button
With so many options available, selecting the right emergency call button requires careful consideration. Here are a few factors to keep in mind:
1. Response Time and Monitoring Services
Some systems connect directly to emergency responders, while others alert family members or caregivers first. Decide which level of response is most appropriate for the user’s situation.
2. Battery Life and Power Backup
A reliable emergency button should have a long battery life, ensuring it remains operational at all times. Some devices also come with backup batteries in case of a power outage.
3. Range and Connectivity
For home-based users, a system with a strong range ensures coverage throughout the house. Mobile users may prefer GPS-enabled buttons that work wherever there is a signal.
4. Ease of Use
The button should be simple to operate, with a clear and responsive design. Complicated features can make it harder to use in an actual emergency.
5. Cost and Subscription Fees
Some emergency call buttons require a monthly subscription for monitoring services, while others operate without ongoing fees. Consider the cost and whether it fits the budget.
The Future of Emergency Call Technology
Technology continues to improve emergency response systems. Newer models come with AI-assisted fall detection, real-time health monitoring, and even integration with smart home devices. As technology advances, emergency call buttons will become even more effective in protecting users.
Conclusion
Emergency call buttons are small devices with a big impact. They provide instant access to help during critical moments, offering safety and reassurance to users and their loved ones. Whether for seniors, individuals with medical conditions, or workers in high-risk environments, these devices serve a vital role in emergency preparedness.
Choosing the right emergency button depends on factors like response time, connectivity, and ease of use. With advancing technology, these devices are only getting smarter, making it easier than ever to stay safe. Ultimately, an emergency call button is more than just a gadget—it’s a lifeline when it matters most.