There’s a moment after a crash when the world tries to move on like nothing happened. Tow trucks come. Cars get dragged away. The lane clears. Traffic flows again. But for the person who got hurt, life doesn’t reset that easily.
Then the insurance call comes. The one that sounds helpful. The one that offers “a quick settlement.”
It can feel like relief. Like a door opening.
Sometimes it’s a door that locks behind you.

Section 1: Why Early Offers Show Up So Fast
Because insurance companies understand human nature. People want the problem to stop. People want bills handled. People want their routine back. People get tired. That fatigue is not a bug in the system, it’s a feature.
An early offer often arrives before you even know what your body is doing. Before the MRI. Before physical therapy shows whether the injury is stubborn. Before you find out that headaches aren’t going away. Before work becomes complicated.
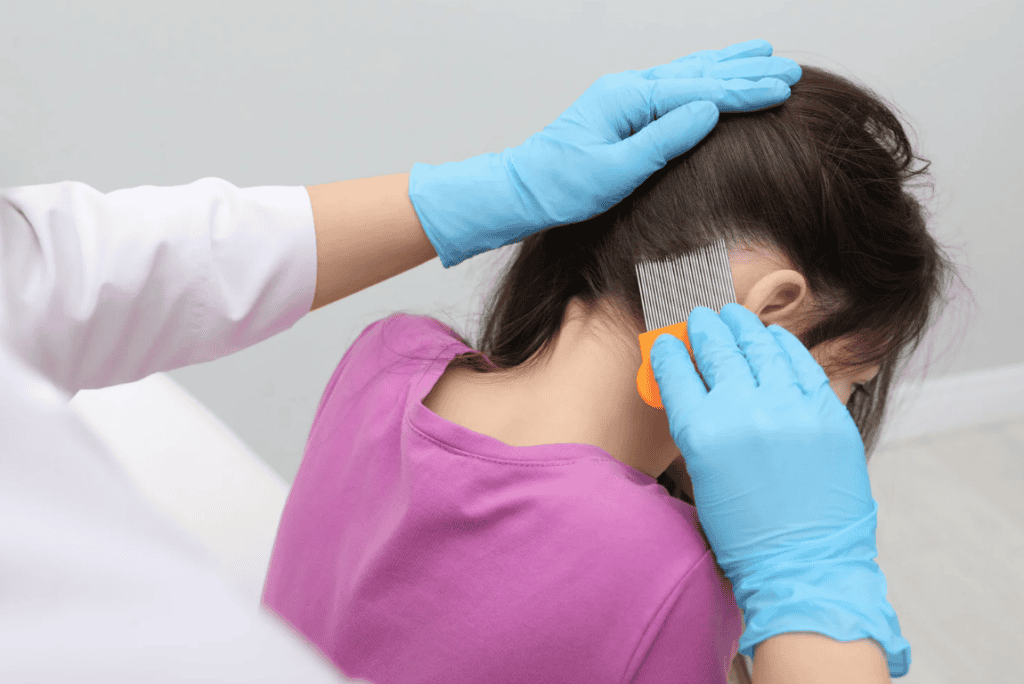
Section 2: Injuries Don’t Always Behave On Your Schedule
A sprain can linger. A back injury can flare up when you sit too long. A concussion can show up as brain fog and irritability instead of dramatic symptoms. Soft tissue injuries can be maddening because they’re real but not always “visible” in a way that satisfies skeptics.
And those skeptics exist. Insurers treat uncertainty like an opportunity to pay less.
That’s why the medical timeline matters. Treatment consistency. Symptom documentation. Follow-ups that show the injury isn’t just a one-day complaint.
Section 3: When Pressure Builds, Structure Beats Toughness
Some people try to muscle through everything alone. They think that’s the “strong” move. But strength doesn’t stop an adjuster from lowballing. Strength doesn’t create medical records. Strength doesn’t calculate future wage loss.
Structure does.
That might mean getting clear guidance early, especially if injuries affect work or fault is disputed. It might mean someone stepping in to protect the claim from being chopped up into convenient pieces. For people who want a crash-focused page that fits naturally right here, accident lawyer belongs in this section where pressure starts to rise.
Section 4: What Makes A Claim “Strong” in the Eyes of the System
It’s not drama. It’s clarity.
- Clear liability evidence: photos, witness statements, consistent reporting
- Clear medical story: diagnosis, treatment plan, documented symptoms
- Clear financial impact: missed work, reduced capacity, out-of-pocket costs
- Clear lifestyle impact: limitations, sleep disruption, daily pain patterns
When those pieces line up, insurers have less room to say “maybe it’s not that bad.”
Section 5: The Mental Side Is Often The Hidden Injury
A lot of people treat anxiety after a crash like it’s embarrassing. It shouldn’t be. The brain has one job: keep you alive. After a collision, it sometimes goes into overdrive.
Suddenly merging traffic feels threatening. Sudden stops feel like a jump scare. Intersections become tense. You might even feel fine until you don’t.
If you want a grounded look at psychological recovery after a collision and why mental healing matters just as much as physical rehab, this article on recovering from a crash from a mental perspective fits naturally here.

Section 6: The Paperwork Game Is Designed To Wear People Down
Insurance claims have a rhythm. Requests for documents. Requests for signatures. Requests for statements. Delays. More requests. “We’re still reviewing.” Then a settlement offer that feels like it’s supposed to be the end.
It’s exhausting. That’s the point.
If you’re tracking your own claim, keep a simple call log: dates, who you spoke with, what was said, what was promised. It doesn’t have to be perfect. Just consistent enough to prevent confusion later.
Section 7: A Few Things That Quietly Harm Claims
- Waiting weeks to get checked out
- Skipping therapy once you start it
- Posting online about feeling “better”
- Taking a settlement before diagnosis stabilizes
- Handing over broad authorizations without understanding scope
None of these are moral failures. They’re normal human choices made under stress. But they can have consequences.
Section 8: A Better Way To Think About Settling
A fair settlement should match the real cost of the injury. Not the hopeful cost. Not the “maybe it’ll go away” cost. The real cost.
That includes future treatment if it’s likely. It includes wage impact if work is affected. It includes the daily-life disruption that doesn’t show up on a receipt but still matters.
The goal is not to drag things out for sport. The goal is to avoid closing the door while the injury story is still being written.
Because once the release is signed, the story doesn’t get edited later. Even if the pain does.