Most people think of the mind as something that reacts to life.
Stress happens.
Emotions follow.
Burnout appears out of nowhere.
Eastern psychology takes a different view. Instead of treating mental states as random reactions, it describes the mind as being shaped by three forces that are always active—competing, blending, and shifting throughout the day.
In classical Indian psychology, the three forces that shape your mind are called sattva, rajas, and tamas.
But you don’t need Sanskrit to understand them.
In modern terms, they can be understood as:
- Clarity (Sattva)
- Drive (Rajas)
- Inertia (Tamas)
Everyone has all three. The question is not which one you have, but which one is currently running the system.

1. Clarity (Sattva): The Balanced Mind
Clarity represents the mind when it is stable, alert, and calm at the same time.
This is not a passive state. It’s the mental mode where:
- Thoughts are organized
- Decisions feel proportional
- Emotions are present but not overwhelming
- Focus comes without force
In Western psychology terms, this resembles regulated executive function—the mind can observe, plan, and respond without being hijacked.
How Clarity Shows Up Day to Day
- You feel mentally “clean”
- Tasks feel doable, not heavy
- You can focus without rushing
- You respond instead of react
- You sleep deeply and wake rested
When Clarity Is Dominant
People often describe this state as:
- Feeling grounded
- Feeling “like myself again”
- Having perspective
- Being patient without effort
Importantly, clarity doesn’t mean constant happiness. It means mental coherence.
2. Drive (Rajas): The Activated Mind
Drive is the force of movement, ambition, stimulation, and urgency.
This force is necessary. Without it, nothing gets built, learned, or achieved. Drive fuels:
- Motivation
- Goal-setting
- Competition
- Creativity
- Desire
In modern psychology, this overlaps with sympathetic nervous system activation and performance-oriented cognition.
How Drive Shows Up Day to Day
- Constant thinking
- Strong opinions
- Urgency to act
- Difficulty slowing down
- Feeling “on” all the time
Drive helps you start things.
But it doesn’t help you stop.
When Drive Becomes Dominant
When unchecked, this force often shows up as:
- Anxiety
- Irritability
- Overthinking
- Insomnia
- Burnout
- Restlessness even during rest
Many high performers live here without realizing it. The mind feels productive—but never satisfied.
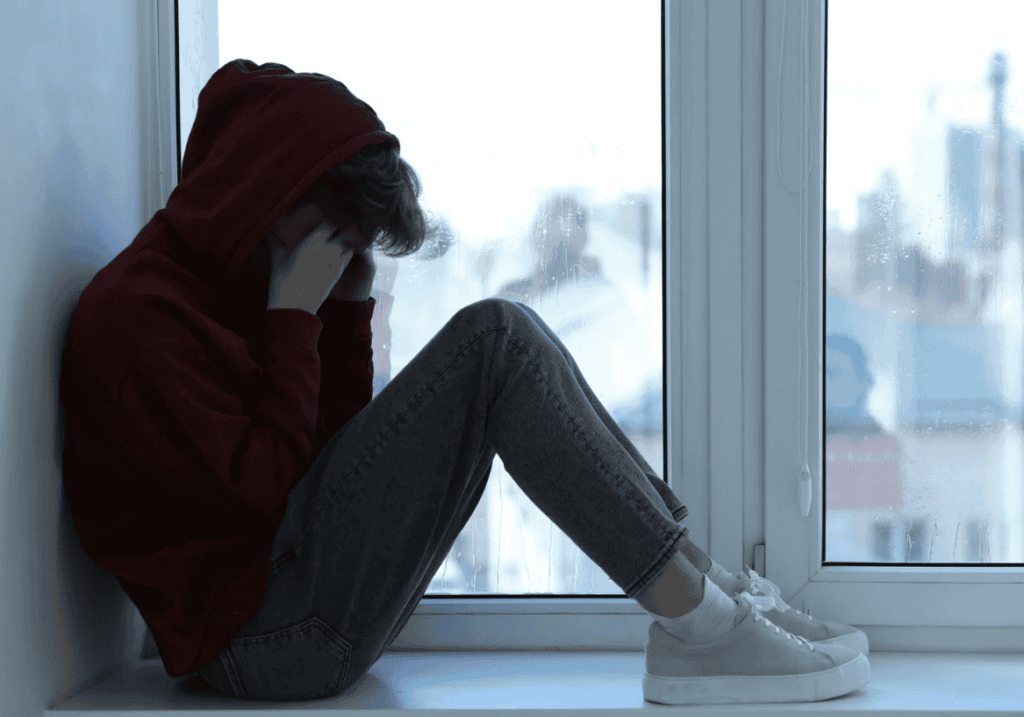
3. Inertia (Tamas): The Slowed or Stuck Mind
Inertia is the force of heaviness, slowing, and withdrawal.
Like the other forces, it serves a purpose. Inertia allows:
- Deep rest
- Sleep
- Recovery
- Conservation of energy
But when inertia dominates the mind, movement becomes difficult.
How Inertia Shows Up Day to Day
- Low motivation
- Brain fog
- Procrastination
- Emotional flatness
- Avoidance
- Excessive sleep or fatigue
This state often feels like:
“I know what I should do—I just can’t start.”
When Inertia Becomes Dominant
People may experience:
- Depressive moods
- Feeling stuck or numb
- Lethargy
- Comfort-seeking behaviors
- Increased sedentary habits
From a psychological lens, this overlaps with hypoarousal, learned helplessness, and reduced dopamine signaling.
The Key Insight: These Forces Are Always Operating
This framework does not label people.
You are not “a tamasic person.”
You are not “a rajasic personality.”
These forces rotate based on:
- Sleep quality
- Diet
- Stress exposure
- Work demands
- Physical movement
- Emotional load
A single day can include all three.
Morning clarity.
Midday drive.
Evening inertia.
Problems arise when one force dominates for too long.
Eastern Psychology vs Western Models
Western psychology often categorizes:
- Disorders
- Traits
- Diagnoses
The Eastern model focuses on:
- State dominance
- Energy balance
- Mental momentum
Instead of asking:
“What’s wrong with me?”
It asks:
“Which force is running my mind right now—and why?”
This subtle shift changes how people relate to symptoms. Anxiety isn’t a flaw. Depression isn’t a failure. Burnout isn’t weakness.
They are signals of imbalance, not identity.
Why This Model Still Matters Today
Modern life strongly amplifies Drive:
- Constant stimulation
- Performance pressure
- Information overload
At the same time, it encourages Inertia:
- Screen fatigue
- Sedentary habits
- Passive consumption
Clarity gets squeezed in between.
Understanding these forces gives people language for experiences they already recognize—but haven’t been able to name.
And naming patterns is often the first step toward changing them.
The Takeaway
Your mind is not broken.
It is dynamic.
At any moment, it is shaped by:
- Clarity (balance and wisdom)
- Drive (movement and intensity)
- Inertia (rest and withdrawal)
Mental health isn’t about eliminating any one force.
It’s about preventing dominance and restoring proportion.
That perspective—rooted in ancient psychology but deeply relevant today—is why these ideas continue to resurface across wellness, neuroscience, and mental health conversations.
Sometimes the most useful frameworks aren’t new. They’re just finally translated into language we can understand.
Rather than treating clarity, drive, or inertia as abstract ideas, Ayurveda looks at how they operate inside a specific person. Exploring Ayurveda online courses or starting with an Ayurveda dosha test can help translate these concepts into something personal and actionable.