Modern dentistry has evolved far beyond basic checkups and cleanings. Today’s dental care focuses on creating comfortable experiences, delivering precise and predictable treatments, and building strong trust between patients and providers. These elements work together to support long-term oral health, reduce anxiety, and make visiting the dentist a more positive part of maintaining overall wellness.
For many families and individuals in Kansas, choosing a trusted provider is an important step toward lifelong oral health. A reliable dentist wichita ks combines advanced tools with a patient-focused approach that enhances comfort, improves outcomes, and fosters trust at every visit.
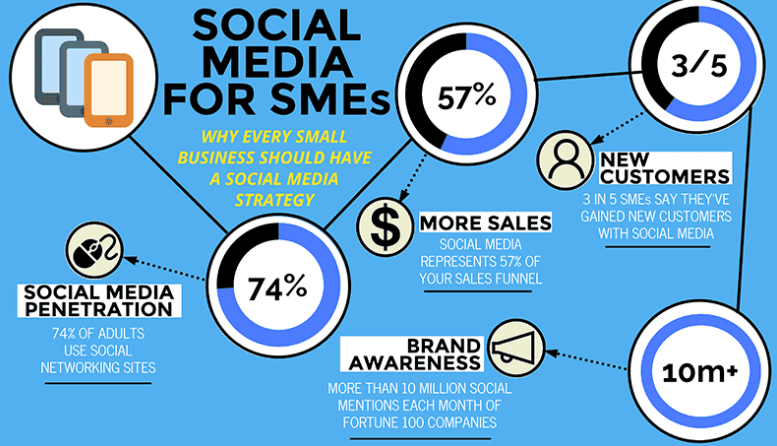
Key Points
- Modern dental technology improves comfort and accuracy
- Precision tools support early detection and better treatment planning
- Patient trust is built through communication and personalized care
- Comfortable visits encourage preventive care and regular checkups
- Modern dentistry supports both oral health and overall confidence

How Technology Has Transformed Dental Care
Advancements in dental technology have changed how oral care is delivered. From diagnostics to treatments, modern tools help dental professionals work smarter and more comfortably. Technology provides clearer insights, supports early detection of problems, and helps dental teams customize care based on each patient’s unique needs.
These advancements not only improve clinical outcomes but also reduce discomfort, shorten recovery times, and make dental visits more efficient and understandable for patients.
Enhancing Comfort Through Innovation
One of the most noticeable benefits of modern dentistry is improved comfort during dental visits. Over the years, dental equipment and techniques have become less invasive and more patient-friendly.
Precision Instruments and Techniques
Advanced tools such as laser dentistry and digital anesthetic systems help reduce discomfort and minimize the impact on surrounding tissues. Procedures that once caused significant sensitivity can now often be performed with greater ease and reduced pain.
Digital Impressions and Scanning
Traditional molds can be uncomfortable for many people. Digital impression technology replaces messy molds with quick scanning techniques that create accurate 3-D images of teeth. These scans are more comfortable for patients and more precise for treatment planning.
Precision in Diagnostics and Treatment Planning
Accurate diagnosis is the first step toward effective care. Modern diagnostic tools help dental professionals detect concerns earlier and more reliably than ever before.
Digital X-Rays
Digital X-rays provide clear images while using less radiation than traditional film X-rays. These high-resolution images allow dental teams to identify decay, bone loss, and other hidden issues that might not be visible during a visual exam.
Intraoral Cameras
Intraoral cameras capture detailed images of the inside of the mouth, allowing patients and providers to view areas of concern on a screen. This transparency enhances understanding and helps dental teams explain recommended treatments with confidence.
How Technology Supports Predictable Results
Once a diagnosis has been made, modern tools help clinicians plan and deliver treatment with precision.
Computer-Assisted Design and Manufacturing (CAD/CAM)
CAD/CAM systems can design and create restorations such as crowns and bridges with exceptional accuracy. This reduces the need for multiple visits and adjustments, helping patients receive stronger and better-fitting restorations sooner.
Laser Dentistry
Lasers can be used for a variety of dental procedures, from cavity removal to gum reshaping, often improving accuracy and reducing recovery time. The precision of laser treatment contributes to better clinical outcomes and enhanced patient comfort.
Building Patient Trust Through Communication
Patient trust is a cornerstone of effective dental care. Technology can enhance trust, but clear communication and personal connection are equally critical.
Explaining Conditions and Options
Modern dentistry use visual tools and detailed images to help patients understand their oral health. When patients can see what a dentist sees, it becomes easier for them to make informed decisions about their care.
Listening and Responding
Patient-focused practices take the time to listen, answer questions, and explain treatment choices in ways that patients can understand. This respectful approach builds confidence and reduces anxiety.
Promoting Preventive Visits and Long-Term Well-Being
Comfort and trust encourage patients to attend regular dental visits. When visits are positive and pain-free, patients are more likely to return for preventive care. Routine checkups help catch concerns early, maintain gum health, and monitor changes over time.
Consistent preventive care is key to long-term oral health. Regular visits allow dental professionals to track patterns, provide personalized guidance, and reinforce healthy habits that support strong teeth and gums.

The Impact on Confidence and Daily Life
Healthy teeth and gums influence daily comfort, social interactions, and quality of life. When patients feel confident in their oral health and the care they receive, they are more likely to enjoy smiling, eating comfortably, and engaging with others without hesitation.
Modern dentistry helps patients achieve this confidence by combining:
- Comfortable experiences
- Precise, reliable treatments
- Clear communication and support
- Trusting partnerships between patients and providers
Frequently Asked Questions
How does modern dental technology make visits more comfortable?
Advanced tools reduce discomfort, shorten treatment times, and often replace older, more invasive methods with gentler options.
Are digital X-rays safer than traditional X-rays?
Yes. Digital X-rays use less radiation and provide clearer, more detailed images than traditional film X-rays.
How does precision technology improve treatment outcomes?
High-resolution imaging and computer-guided systems allow dental professionals to plan and deliver treatment more accurately, leading to better-fitting restorations and more predictable results.
What can I do to feel more comfortable during dental visits?
Communication with your dental team about your concerns and preferences helps them tailor care to your needs. Modern technologies also improve comfort for many procedures.
Why is trust important in dental care?
Trust encourages patients to attend regular visits, follow recommendations, and maintain long-term oral health, leading to better outcomes and more positive experiences.