Construction work keeps growing in New York City every day.
- New buildings rise
- Roads get repaired
- Old structures get replaced
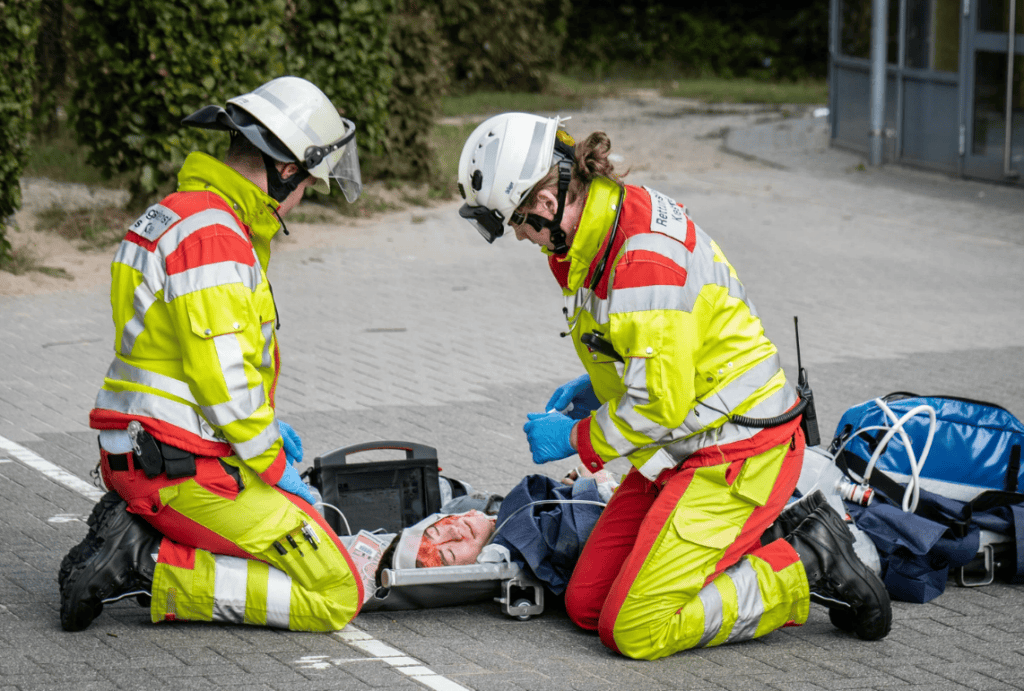
But construction sites can also be dangerous places. You can face serious risks while working near heavy equipment and tall structures.
Construction accidents can happen more than most people realize. Certain injuries are minor. Others may radically transform your life. When you understand the major causes of construction accidents in New York City – you can be vigilant and defend your rights after an injury.
This guide will explain the main reasons why construction accidents happen and what you should know if you get hurt.

Falls From Heights
Falls are one of the biggest causes of construction injuries. Many workers perform tasks on:
- Scaffolds
- Ladders
- Roofs
- Elevated platforms
These areas place you high above the ground. One mistake can lead to a serious fall.
Falls often happen because of:
- Missing safety harnesses
- Broken ladders
- Unstable scaffolding
- No guardrails
- Slippery surfaces
A fall from height can cause broken bones or head injuries. It can also lead to spinal damage. In many situations, proper safety equipment could prevent construction accidents. When safety rules are ignored, workers get hurt.
Falling Objects and Debris
Construction sites have tools and materials placed at different levels. Objects may fall from above if they are not secured properly.
You may get injured by:
- Loose building materials
- Falling tools
- Demolition debris
- Equipment parts
- Loads moving from cranes
Even a little thing can result in catastrophic damage if it falls from a height. Head injuries are common. Hard hats help – but accidents still happen when safety rules are not followed.
Machinery and Equipment Accidents
Construction work depends on heavy machines such as:
- Cranes
- Forklifts
- Bulldozers
- Power tools
These machines can help you complete your projects faster. They can also cause serious injuries if you use them in wrong ways.
Equipment accidents happen because of:
- Poor maintenance
- Lack of worker training
- Machine malfunction
- Operator mistakes
- Missing safety guards
You can suffer from crushing injuries or serious wounds. Some accidents can also result in lifelong harm. Regular inspections and thorough training limit danger – although failures can still occur.
Electrocution Hazards
Construction workers must also operate near electrical systems. Contact with live wires might result in severe injuries or death.
Electrocution occurs due of:
- Exposed wiring
- Faulty equipment
- Improper grounding
- Overhead power lines
- Wet work areas
Electrical injuries may result in burns and nerve damage. They may also have an effect on your heart. These mishaps are often avoidable with careful preparation and protective equipment.
Slips, Trips and Same-Level Falls
Not every accident involves heights. Many accidents happen on the ground due to dangerous walking conditions.
Common hazards include:
- Wet floors
- Loose cables
- Uneven surfaces
- Tools left on the ground
- Poor lighting
A minor trip may result in significant injury. You may get fractures or back issues. Clean work environments and warning signs may help avoid these mishaps.
Trench and Structural Collapses
Excavation work is common on construction sites. Workers mostly enter trenches to perform underground tasks. These areas can become dangerous if not supported properly.
Trench accidents may happen due to:
- Weak support systems
- Loose soil
- Poor planning
- Water buildup
- Heavy equipment near edges
A collapse can trap workers under heavy material. These accidents can cause severe injuries. Safety inspections and protective systems are required – but violations still happen.
Exposure to Dangerous Materials
Construction sites contain harmful substances. Workers may handle chemicals and toxic materials during daily tasks.
You may face exposure to:
- Asbestos
- Lead
- Chemical solvents
- Paint fumes
- Silica dust
Long-term exposure may result in respiratory issues or severe sickness. Protective equipment and ventilation may assist to lessen the danger. But unsafe handling still causes injuries.
Lack of Safety Training
Many accidents happen because workers do not receive proper training. Construction work involves complex tools and procedures. Without clear instructions, mistakes happen easily.
Poor training may lead to:
- Wrong equipment use
- Ignoring safety rules
- Miscommunication
- Unsafe handling of materials
Employers must provide safety training. When training is limited, workers face a greater risk.

Unsafe Worksite Conditions
Sometimes the worksite itself is unsafe. Poor management increases the chance of injury.
Unsafe conditions may include:
- Missing warning signs
- Poor supervision
- Lack of safety checks
- Broken equipment
- Rushed work schedules
When safety is not a priority, accidents happen more often.
Human Error and Fatigue
Construction work is physically demanding. Long hours and heavy tasks reduce concentration.
Human factors include:
- Worker fatigue
- Poor communication
- Distraction
- Lack of rest
- Stress
Proper scheduling and supervision help reduce these risks.
Why Construction Accidents Still Happen
You may wonder why accidents continue even with safety rules. Many projects follow tight deadlines. Some companies ignore safety to save time or money.
Common reasons include:
- Pressure to finish work quickly
- Weak safety enforcement
- Poor planning
- Lack of equipment maintenance
- Failure to follow regulations
These problems increase injury risk.
How Construction Accidents Affect Your Life
A construction accident can affect your entire life. You may face medical bills and lost income. Recovery may take months. Some injuries cause permanent limitations.
Common effects include:
- Medical expenses
- Missed work
- Physical pain
- Reduced ability to work
- Long recovery
Because of these consequences, many injured workers seek legal counsel.
During this procedure, some individuals speak with construction accident attorney NYC to learn more about how injury claims operate and how compensation is determined.
What You Can Do After a Construction Accident
If you get injured, quick action can protect your health and your claim.
You should:
- Seek medical treatment immediately
- Report the accident
- Document the scene
- Collect witness information
- Keep medical records
These steps help create strong evidence.
How Safety Measures Help Prevent Accidents
Most construction accidents can be prevented. Proper safety practices reduce risk.
Important safety steps include:
- Wearing protective gear
- Following safety rules
- Maintaining equipment
- Reporting hazards
- Providing worker training
When safety rules are followed, job sites become safer.
Final Thoughts
Construction activity contributes to the expansion of New York City. It also poses considerable hazards. Many accidents occur as a result of:
- falls
- equipment failures
- falling items
- risky situations
Basic safety measures may have stopped a lot of these injuries from happening.
You can better protect yourself if you know about these dangers. You may be able to take legal action if there is an accident on the job. Knowing what causes accidents may help you protect your health, safety, and future.