Addiction is a problem that weaves through the physical, emotional, and social domains of one’s life. It thus demands a treatment philosophy that is as holistic as it is compassionate.
Rather than the general pathways into recovery discussed in most writings, this article assumes a somewhat different angle in digging into strategies for effective addiction treatment that are not generally discussed, along with newer innovations that promise lifelong success.
Understanding Addiction Beyond the Surface
Traditionally, addiction has been misconstrued as a willpower problem when it is a chronic disease founded on genetics, psychology, and environmental causes. Understanding these layers goes a long way toward devising effective treatment strategies.
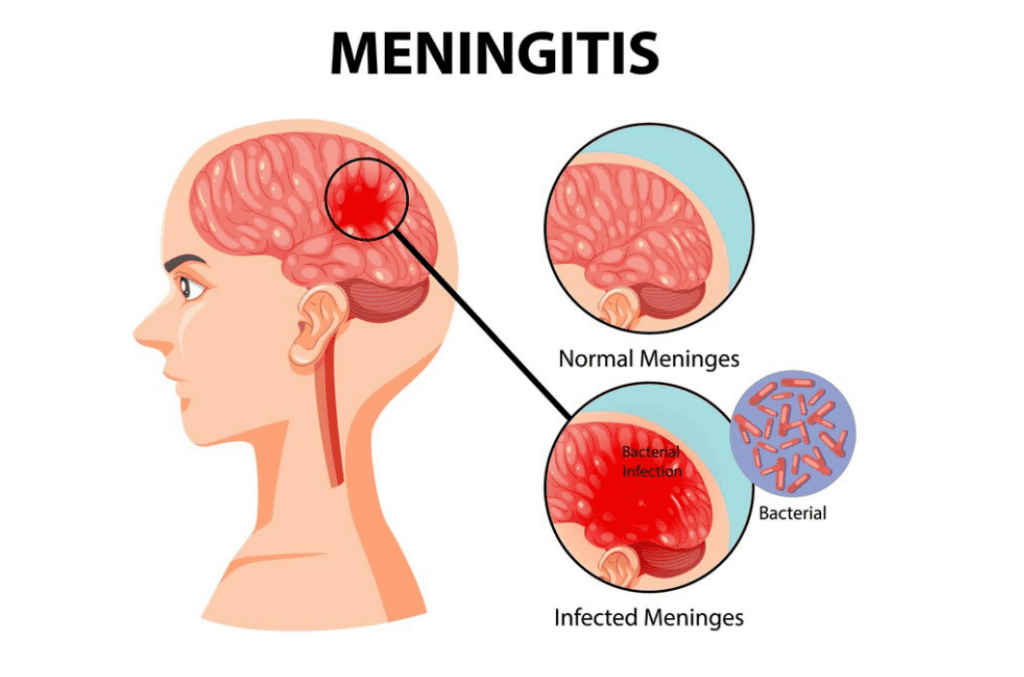
1. The Role of Neurology
Substance use changes brain chemistry, mainly in areas related to reward, decision-making, and impulse control. It, therefore, becomes an ever-hard task for the individual to stop using substances without professional medical or therapeutic intervention.
2. Social and Emotional Triggers
Social isolation, trauma, and stress are major predisposing factors in addiction. Identifying them will help the individual or his support network find practical ways to avoid recurrence.
Innovative Strategies for Effective Addiction Treatment
While more traditional means, such as detox and counseling, remain very effective, modern times have brought about new tools in recovery.
1. Virtual Reality Therapy
Some facilities are now using Virtual Reality to re-create simulated triggering situations safely. This allows them, in real-time and sans relapse, to practice coping mechanisms.
2. Biofeedback Techniques:
Many biofeedback devices monitor physiological responses regarding heart rate, muscle tension, etc. By understanding their signs of stress, individuals can learn how to cope with cravings better.
3. . Mobile Apps for Recovery
Today, there are mobile apps for daily journaling, a meeting locator, and tracking one’s progress so individuals can stay connected to their goals and support groups.
The Importance of Dual Diagnosis Treatment
For many, addiction does not occur in a vacuum. Co-occurring mental health disorders, such as depression or anxiety, may serve to fuel substance abuse.
1. Co-occurring Disorders Identified
In-depth diagnoses facilitate the discovery of profound mental health problems that need to be taken care of along with addiction. Without consideration, incomplete recoveries arise.
2. . Integrated Treatment Plans
Dual diagnosis programs address addiction treatment along with other concurrent mental health disorders. Many times, psychiatric interventions, medication, and sometimes therapy make up these facilities.
The Magic of Holistic Cure
Unlike conventional therapies, holistic treatments align the mind, body, and soul.
1. Yoga and Meditation
These practices help heighten awareness, reduce stress, and equip the individual with ways to counteract cravings and emotional storms.
2. Nutritional Rehabilitation
Abuse of substances often leaves the body bereft of essential nutrition. Personalized nutrition may facilitate recovery of physical strength and clarity of the mind.
3. Art and Music Therapy
These creative outlets allow clients to work through their emotions and build self-esteem without feeling intimidated. Many people can discover new passions and positive outlets through these types of therapies.
Community-Based Recovery Models
Community support has become one of the key features in recovering from addiction, either entirely or partially, as it offers some sense of belonging and personal accountability.
1. Peer-Led Recovery Groups
Other support models are provided by groups like SMART Recovery and Refuge Recovery; these differ from more traditional 12-step programs, offering empowerment and evidence-based approaches.
2. Community-Based Programs
The various community-based activities mainly comprise workshops, job training, and recreational programs that further help the individual build back his or her life and integrate himself/herself into society.
3. The Family’s Part in Recovery
Family members are very much a part of the recovery process. Teaching families about addiction and including them in therapy sessions may help reinforce support systems and heal broken relationships.

Overcoming Stigma: Changing the Conversation Around Addiction
Stigma remains one of the single largest barriers to treatment. A shift in public perception can help more people seek out treatment without fear of judgment.
1. Education and Advocacy
Public campaigns on addiction as a disease, not a moral failure, are necessary to help overcome stigma.
2. Success Stories
Stories of recovery from walks of life give addiction a face and ensure recovery is possible in any person’s life.
3. The Language Matters
Using such terms as “person with substance use disorder” instead of “addict” conveys empathy and respect.
Treatment customized to individual needs
Recovery is different for everyone, and treatment plans are often structured to meet the particular circumstances and struggles of the individual.
1. Gender-Specific Programs
Some facilities have programs that address either the specific experiences of men or women and, as such, focus on gender-specific triggers and societal pressures.
2. Cultural Competency in Treatment
Cultural beliefs and practices shape perceptions related to addiction and recovery. Programs that respect and integrate these elements usually report higher success rates.
3. Long-Term Recovery Plans
A well-structured aftercare plan that includes therapy and support groups keeps the individual on the right track even after finishing the initial treatment.
Making Use of Outpatient Programs for Lasting Recovery
Outpatient programs offer flexibility for people to recover while continuing their daily life. They provide structured therapy sessions without needing to stay in residence.
1. Balancing Recovery and Everyday Life
Outpatient programs are best for those who have commitments toward work, school, or family. They will get the tools to handle situations better in the real world to maintain sobriety.
2. Continuing Care
Treatment in this outpatient addiction treatment center will provide one with continued care and counseling for motivation and to keep one on track.
3. Transitioning from Inpatient Care
Outpatient programs usually serve to bridge the gap between one who has been undergoing some intense inpatient care and independent living.
The Role of Technology in Recovery
Technology is changing the face of addiction treatment: support is becoming more accessible and tailored.
1. Teletherapy Services
Online therapy sessions may translate into a person getting counseling while still in the comfort of one’s home without any sort of geographical barrier.
2. Wearable Devices
Wearable devices that track physiological and emotional states enable notification when intervention may be necessary, both for the individual and their support networks.
3. Virtual Communities
Scanning online forums and social media groups provides 24/7 access to peer support in developing a sense of connection and accountability.
Wrapping Up
Recovery from addiction is one of the most challenging tasks because it demands creativity, community, and personalization. With investigations into holistic therapies, using technology to facilitate treatment and outpatient solutions, one lays a solid foundation for building long-term sobriety.
Facilities such as this outpatient addiction treatment program offer a greatly needed resource for anyone who is in need of a flexible, supportive path toward recovery. No matter how bad things get, anyone can be free from their addictions if they have the will and the right tools.