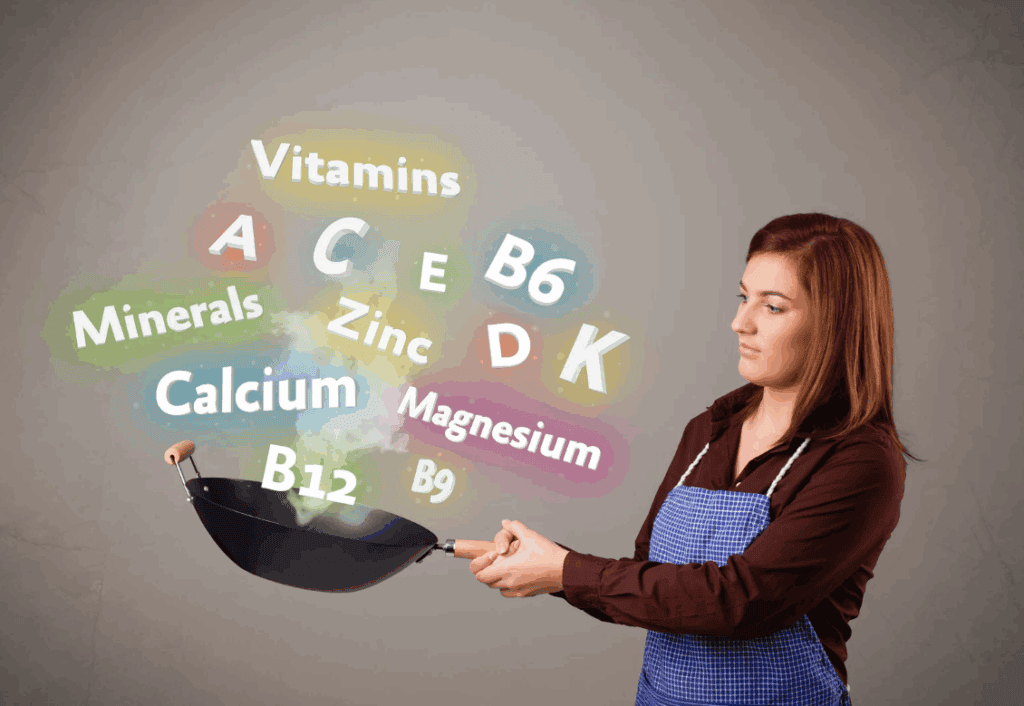
As women age, particularly during and after menopause, their nutritional needs change significantly. Hormonal fluctuations, reduced nutrient absorption, and an increased risk of chronic conditions can all affect your health. When addressing menopause and the sudden shifts, proper nutrition becomes more important than ever.
Many formulas marketed as women’s vitamins now include essential nutrients designed to support bone health, hormonal balance, and overall vitality during this transition. By learning which vitamins and minerals are vital during aging, women can make informed choices and potentially mitigate the effects of menopause as they grow older.
Vitamin D and Calcium: Core Nutrients for Bone Health
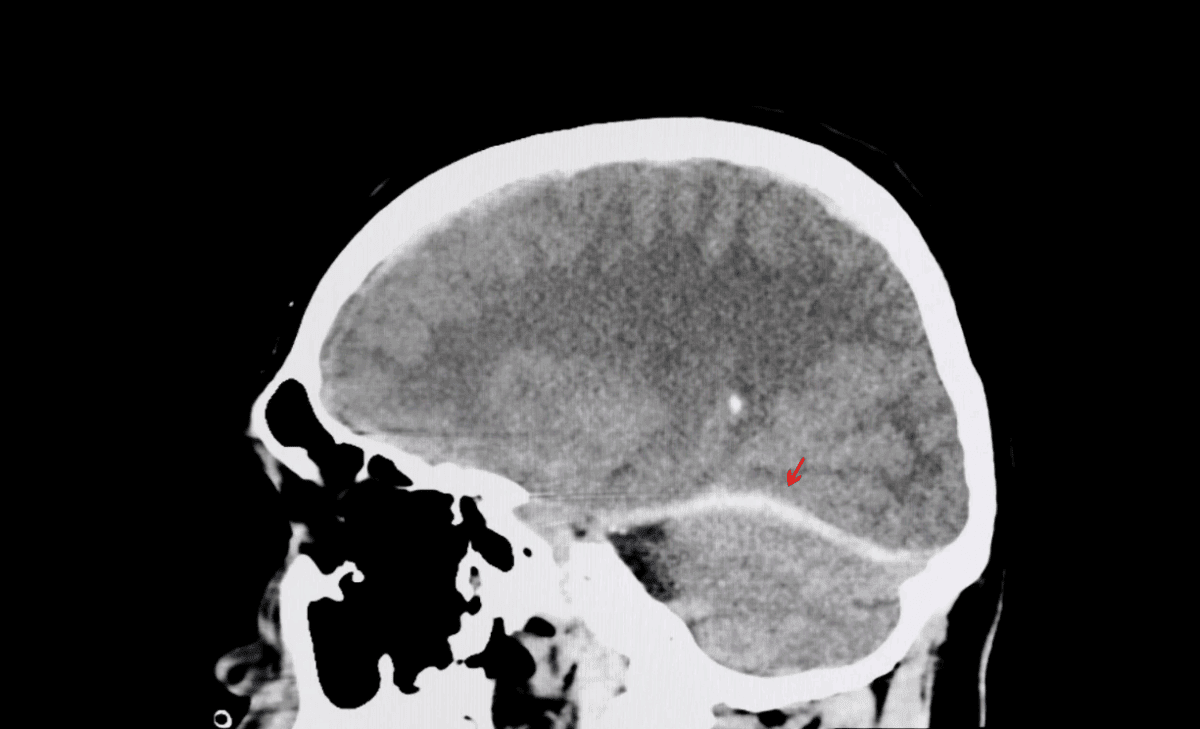
Vitamin D and calcium are two of the most important nutrients for bone health, especially during menopause and beyond. As estrogen levels decrease, women become more susceptible to osteoporosis and bone density loss. Vitamin D helps with calcium absorption, which is essential for maintaining strong, healthy bones.
After menopause, the body’s ability to process vitamin D may decline, making supplementation increasingly useful. Daily intake recommendations vary by age and health status, but most women over 50 should aim for 1,200 milligrams of calcium and 600 to 800 IU of vitamin D.
Natural sources of vitamin D include fatty fish, fortified dairy, and sunlight, while dairy products, leafy greens, and fortified foods are good sources of calcium. Incorporating both nutrients into your daily routine can help prevent bone weakening and fractures.

Vitamin B12: Supporting Energy and Cognitive Function
Vitamin B12 plays a vital role in maintaining energy levels, supporting cognitive function, and producing red blood cells. As women age, their ability to absorb vitamin B12 from food decreases due to reduced stomach acid production. This can lead to deficiencies, which may cause fatigue, cognitive decline, and nerve damage.
B12 deficiency is especially common among those who follow a vegetarian or vegan diet, as B12 is mainly found in animal products. The recommended daily intake is 2.4 micrograms, but older adults may need higher amounts, particularly if absorption is impaired.
Supplementing with B12 through fortified foods or supplements can help combat deficiencies and maintain energy levels, cognitive health, and overall well-being. Women should consult with a healthcare provider to determine the best approach for their specific needs.
Vitamin E and Antioxidants: Combating Cellular Aging
Another potent antioxidant that lends a hand in protecting your skin and cells from oxidative stress is vitamin E. As women get older, their bodies’ ability to combat oxidative damage decreases, leading to fine lines, wrinkles, and other signs of skin aging.
Vitamin E helps mitigate this by neutralizing free radicals, unstable molecules that can damage cells. It also supports immune function and may improve skin hydration and elasticity. While vitamin E is found in foods like nuts, seeds, and vegetable oils, supplementation should be approached with caution, given that high doses can interfere with blood clotting.
Vitamin K2: A Lesser-Known Nutrient for Heart and Bone Health
Vitamin K2, often overshadowed by vitamin K1, is significant in calcium regulation, bone health, and cardiovascular well-being. Research suggests that vitamin K2 helps direct calcium to bones and teeth while preventing it from accumulating in the arteries, potentially reducing the risk of arterial calcification and cardiovascular disease.
This nutrient is especially important after menopause, when estrogen levels drop and bone health becomes a concern. Vitamin K2 is found in fermented foods like natto, hard cheeses, and egg yolks, and supplementation may be beneficial for women looking to improve their bone strength and heart health as they age.

What Are Some Menopause-Specific Considerations?
Hormonal shifts during menopause can lead to a range of symptoms, including hot flashes, mood swings, sleep disturbances, and changes in metabolism. Vitamins and minerals play a key role in addressing some of these issues.
Vitamin B6, for example, helps regulate mood and reduce irritability, while magnesium supports muscle relaxation and sleep. Meanwhile, vitamin D is crucial for hormonal balance and managing the effects of decreased estrogen, particularly in supporting bone density and cardiovascular well-being.
What’s more, menopausal women may experience changes in metabolism, increasing their risk of weight gain. Vitamins like B12 and magnesium can help maintain energy levels and support metabolic processes. Addressing these deficiencies with targeted supplementation can help reduce the severity of your symptoms and promote overall wellness during menopause.
Nourish Wellness Through Every Stage of Life
Proper vitamin intake is critical to addressing the unique health challenges of aging and menopause. By prioritizing nutrients like vitamin D, B12, and E, women can enhance their bone health, energy levels, cognitive function, and overall vitality.
With informed choices and balanced supplementation, it’s possible to age gracefully and maintain optimal health. The right vitamins can help women feel their best during every stage of life.